Release date: 2015-03-02
HIV, the human immunodeficiency virus, has been working for the first time since its discovery in the United States in 1983. Among them, HIV vaccine combined with gene therapy is a very important and promising direction in many studies. The development of the HIV vaccine has experienced a lot of ups and downs, and recently, the Farzan team from the Scripps Research Center has made remarkable progress in this area, which has once again aroused people's attention in this field.
So why is it difficult to develop an HIV vaccine? How do scientists overcome these difficulties? How is gene therapy combined with vaccine development? This inventory takes you through the history of the development of HIV vaccines through genetic engineering and the latest breakthroughs.
[1] Why is it difficult to develop an HIV vaccine?
First, there are many variants of HIV, and it is difficult for vaccines to be universal. The HIV virus is divided into two subtypes (HIV-1, HIV-2), and even if the virus of the same subtype is in different patients, the virus strain is different. The vaccines or antibodies developed in the laboratory for a strain are often not clinically applicable to all patients.
Secondly, the traditional method of developing vaccines through active immunization does not work. The classic way to develop vaccines is to use all or part of the inactive virus to induce immunity, but the HIV effort has hidden most of the external structures that are easily recognized by antibodies. Therefore, it is very difficult to find a molecule that can stimulate the body's immune response while also fighting various mutations of the virus.
The following highlights three more important research teams to review the development of HIV vaccine gene therapy by reviewing their research.

[2] Philip Johnson team: an imaginative start
Since it is impossible to induce immunity by active immunization, passive immunization and frequent injection of antibodies are not realistic. Then, whether the genes expressing HIV antibodies are introduced into the human body in some way, so that these genes continue to express antibodies. So cleverly spare people's own immune system, so that people get immunity? This imaginative idea was put forward and tried as early as 2002.
Philip Johnson, a pediatrician at the Children's Hospital in Philadelphia, Pennsylvania, and his team published a paper in the Journal of Virology titled Generation of Neutralizing Activity against Human Immunodeficiency Virus Type 1 in Serum by Antibody Gene Transfer: They Extracted from AIDS Patients A small amount of monoclonal antibodies that neutralize a large number of HIV-1 viruses. Next, the gene expressing these antibodies is introduced into an adeno-associated virus (AVV) which is non-toxic to the human body, and the thus-modified AVV virus is injected into the muscle cells of the mouse. Six months later, a higher concentration of HIV neutralizing antibodies was detected in the serum of the mice.
Conclusion 1: This study demonstrates that adeno-associated virus AVV can be used as a vector to introduce antibody genes into humans. At the same time, after injecting into muscle cells, the expressed antibody protein can enter the bloodstream. In this way, we can bypass the human immune system and endogenously express large amounts of HIV neutralizing antibodies.
Well, the problem is coming. Is the antibody expressed in this way sufficient for the body to produce immunity against HIV? Then, the Johnson team conducted a second important experiment and published the results in Nature in 2009. This time, they selected an HIV-like virus, the SIV virus, in the rhesus monkey to conduct experiments. In antibody selection, Johnson spliced ​​naturally extracted antibodies to form an antibody molecule called immunoadhesin, which maintains a certain level of concentration in the human body. Like the first time, the researchers introduced the gene encoding the immunoadhesin into AVV and injected it into monkeys. Four weeks later, when the researchers injected SIV virus into monkeys from 9 experimental groups (injected with modified virus) and 6 controls (without any treatment), 6 monkeys in the experimental group were not infected. Six of the control group of monkeys were all infected with SIV.
Conclusion 2: The method of transducing genes by adeno-associated virus AVV can make the body obtain immunity.
The results were delighted, but they also raised new questions for us:
1. There are three monkeys in the experimental group who did not gain immunity in this way, and the specific reasons are not clear.
2. It is not clear how long the adeno-associated virus AVV can survive in the organism, and this is closely related to whether the vaccine can make people have long-term immunity. Once the adeno-associated virus AVV is completely killed or inhibited, the corresponding antibody gene cannot be expressed.
3. There is also a potential problem: antibody molecules expressed by antibody genes may cause the immune system to respond, which not only limits the effectiveness of the treatment, but may also lead to more serious consequences.
4. Finally, the SIV virus is very, very sensitive to antibodies compared to HIV. Therefore, it is still a big unknown whether we will use the animal model of HIV to repeat the test.
(The picture shows the Nobel Prize winner virologist David Baltimore)
[3] Baltimore team: further optimize the experimental technology, successfully let the mouse immunize the HIV virus
To answer these questions, the famous biology professor at the California Institute of Technology, the Nobel Prize-winning virologist David Baltimore and his team did further research based on Johnson's work and put Johnson's ideas in HIV-infected. More specific practice and optimization have been done on mice. Blatimore calls this method a plasmidized immune defense (VIP: Vectored Immunoprophylaxis):
First, Baltimore was selected for further optimization on the gene vector. He chose a special adeno-associated virus AVV, which has the ability to survive in vivo for a long time and express the ability to express the gene encoding the antibody continuously. It has the basis for providing long-term immune protection for living organisms. Secondly, in the selection of HIV neutralizing antibodies, the emergence of more antibodies against HIV from 2002 to 2011 has given Baltimore more choices. He tested it on mice with a human immune system. The effect of 5 different antibodies, one at a time.
The results are quite gratifying: of the five different antibodies, two antibodies named b12 and VRC01 proved to work well. Even mice receive a 100-fold higher dose of HIV than natural infections. After 52 weeks, antibody expression levels remained high, indicating that a single dose can provide lasting protection.
Conclusion 3: Baltimore's experiments show that mammals can obtain immunity against HIV through this gene therapy. Moreover, HIV antibody expression levels can last for a long time, which will prepare for the human trial phase.
[4] Farzan team: designing efficient artificial proteins
The HIV vaccine was developed by genetic engineering: the Johnson team should be said to be the pioneer to provide basic experimental ideas and technical processes for future research, and Baltimore further applied this technology to mammals and obtained it. The immunity to HIV. Then Farzan's work is even further:
They designed a new anti-HIV protein molecule based on the process of HIV virus infection: eCD4-lg. This synthetic protein has a stronger immune protection than other molecules produced by the human body under natural conditions.
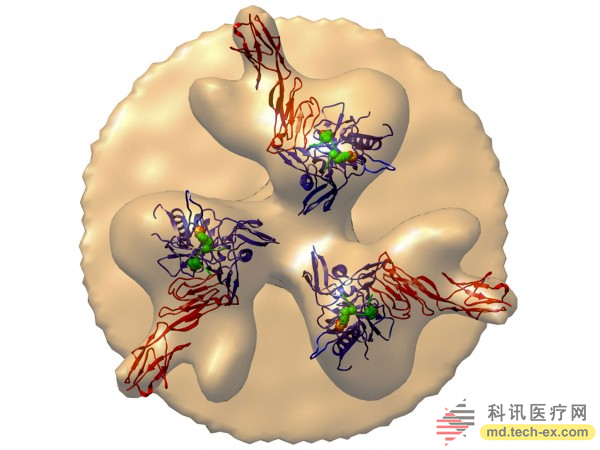
Briefly describe the process by which the HIV virus infects cells: the HIV virus infects cells by sequentially binding to two receptors on the surface of the leukocyte. First, the HIV glycoprotein glycoprotein gp120 binds to the CD4 receptor of leukocytes. This combination distorts the gp120 protein and exposes a further portion of the surface of the virus to bind to another receptor, CCR5, on the surface of the leukocyte. The newly constructed protein eCD4-lg of Farzan et al. is composed of a part of two receptors of CD4 and CCR5 linked to the same antibody. In this case, when the AIDS virus and eCD4-lg are combined, the virus can no longer infect the cells, thus realizing the neutralizing effect of the eCD4-lg protein on the virus.
Experiments carried out in test tubes showed that eCD4-lg has a stronger ability to prevent viral infection of cells than all known natural HIV antibodies. To test whether eCD4-lg is effective in animals, the investigator put the gene encoding eCD4-lg into a non-toxic virus and infected four experimental groups of monkeys with this engineered virus. After injection of the modified virus, a large number of eCD4-lg proteins were produced in 4 monkeys. For the next 34 weeks, the researchers injected a continuous, high-dose AIDS virus into the four monkeys in the experimental group and four monkeys in the control group (without eCD4-lg gene injection). As expected, the monkeys in the experimental group were not infected with AIDS, and none of the monkeys in the control group were spared.
In summary, the artificially designed antibody eCD4-lg has the following advantages:
1. There is no obvious immunological rejection of eCD4-lg in animals. It is predicted that this protein is too similar to the cellular components in the body. On the contrary, HIV neutralizing antibodies used by researchers previously lead to varying degrees of immune rejection.
2. Experiments carried out in test tubes showed that eCD4-lg has a stronger ability to prevent viruses from infecting cells than all known natural HIV antibodies.
3. In theory, the HIV virus is less susceptible to mutation when combined with eCD4-lg than the broad-spectrum neutralizing antibody bNAb, because the HIV virus binds to the two receptor portions of CD4 and CCR5 in the protein. .
4. More importantly, eCD4-lg is tightly bound to glycoproteins in conserved regions of the HIV virus membrane. This means that it is well-prepared and can cope with multiple strains of different HIV subtypes.
Of course, there are many voices in the scientific community that question the eCD4-lg:
Baltimore noted that this new development only provides data on test tubes and animal experiments. Therefore, he added: "Maybe eCD4-lg is indeed a better molecule than natural HIV antibodies, but whether it can work in patients or not is a big problem to be solved. In clinical, you are very It's hard to predict what will happen. "It's important to note that the Baltimore team and the Johnson team's respective AIDS gene therapy have already entered clinical trials.
Johnson holds the same view: eCD4-lg does not necessarily have a better effect in the human body than bNAbs. At the same time, he also put forward another view: compared to eCD4-lg, the ability of HIV natural antibodies to resist viruses may be slightly weaker. However, these natural antibodies may be enough to contain HIV. "How good is the drug (no drug)? No one knows the specific degree. So, as long as the treatment we use can effectively prevent the disease from happening."
In response to these questions, Farzan said that he has begun to plan related experiments, trying to fully test the effectiveness and role of eCD4-lg before entering clinical trials to ensure that no unexpected situation.
[Conclusion]
The road to scientific development has never been a road to prosperity. Before combining the gene therapy to study HIV vaccine, many scientists have devoted themselves to other methods of developing vaccines, invested huge human and material resources, and even progressed to the early stage of clinical research, and ultimately they ended up failing, which made people sigh. (For specific examples, please refer to Merck's "STEP"). More often, what we often see is that the glaring news headlines that once succumbed to AIDS are slowly being forgotten.
However, hope always exists. Through a series of reviews, we can see that the development of HIV vaccine through genetic engineering is still a promising path, at least for now. As mentioned above, the research of the Johnson and Baltimore team has already entered the news of the clinical trial period, and it is full of expectations for the cure of AIDS. At the same time, we also noticed the huge potential danger of gene therapy. The human body can't immune to the inserted gene. It is difficult to predict whether these antibody genes introduced into the human body will have other unknown effects. Therefore, we need to step by step and carefully test the argument. Difficulties are great, but scientists will not give up hope. We also have reason to believe that, like many times in history, one day, humans will ignite the flaming Prometheus fire and win this battle with the virus.
Best Neck Massager,Shiatsu Neck Massager,Neck Relax Massager,Best Massage For Neck Pain
Shenzhen Jie Zhong Lian Investment Co., Ltd. , https://www.meizons.com